
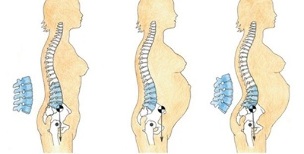
The elderly, professional athletes, as well as those whose occupations involve sitting for a long time or standing on their feet, are often prone to various diseases of the musculoskeletal system. Irrational daily menu, physical inactivity causes thirst, bone and cartilage destruction. As a result, osteochondrosis of the lumbar spine occurs, its symptoms and treatment depend on the personal characteristics of the organism, as well as the severity of the lesion.
According to the 10th revised international disease classification, the disease is coded M42. Sometimes patients are given a complicated diagnosis, coding simplifies the work of the doctor. This short alphanumeric naming can be recorded in the medical history, outpatient cards. So what is lumbar spine osteochondrosis? What is the cause of its occurrence? What are the manifestations of this disease? This publication tells the whole story.
Causes of lumbar osteochondrosis
Osteochondrosis of the lumbar spine often results in injury and a slow-moving lifestyle. Among other things, one of the main roles played by the burdensome offspring, similar to the hormonal, chemical, psychogenic background of the body.
If parents have lumbar osteochondrosis, the symptoms and treatment tend to manifest and be passed on to their children. After inheriting predisposing factors, offspring are also at risk for this disease.
Provoking factors also include the following reasons for occurrence:
- Other diseases, such as the gastrointestinal tract, liver, pelvis, nervous system;
- Smoothen metabolism;
- Shift of acid-base balance towards oxidation (acidosis);
- Decreased motor energy;
- Stress, nervous state;
- Long awkward posture, incorrect posture.
Often, sacral osteochondrosis occurs as a result of hypothermia, hormonal disorders, or as a result of pathological congenital defects in the spine.
Symptoms of lumbar osteochondrosis
The signs of lumbar osteochondrosis are associated with the fact that the spinal nerve fibers pass through the back area within the spinal canal. Depending on the localization, the severity of the defeat of some roots, the manifestations of the disease vary.
With lumbar spine osteochondrosis, the symptoms are as follows:
- Pain syndrome- most patients complain of lower back pain in osteochondrosis. The pain occurs directly in the zone of violation or radiates to the gluteal region, the sacrum of the foot from the side of the lesion;
- Signs of tension- pain increases with a certain position, but when the position of the body changes, the pain disappears suddenly. The most commonly used test is called the inventor - Lasegue syndrome - the pain increases when a straight limb is lifted upwards, and disappears when the leg is bent at the knee;
- Decreased or increased sensitivity- these symptoms are directly related to damage to the radicular nerve, impaired sensitivity not at the pathological location, but at a certain distance. Patients experience hypesthesia, hyperesthesia or paresthesia, which is characterized by unusual projection sensations, such as goose bumps, tingling, and so on.
Often, with lumbar osteochondrosis, decreased motor activity, this is associated with muscle atrophy of various degrees. In certain circumstances, there are functional limitations, in other cases paralysis and paresis occur.
Also, lumbar chondrosis is associated with damage to the spinal canal, with its irritation and cramps, vegetative changes appear. Blood circulation in the legs slows down, the lower part of the foot is always frozen, there is pale on the skin. Other organs in the lumbar region are often affected. Thus, with damage to the bladder, urinary incontinence develops or, conversely, delays.
Level of disease
- Grade 1 lumbar osteochondrosis is an early type of pathology. It is characterized by low density intervertebral discs. Pain syndrome appears with a sharp turn of the body, after physical exercise or sitting for a long time.
This type of disease is common in drivers, office workers, athletes, and people working in harsh climates. Pain is not characterized by an acute attack, but develops as dull or debilitating pain.
At this stage, people are in no hurry to go to the doctor, but use traditional treatment methods, such as ointments, compresses. This condition leads to the fact that osteochondrosis of the lumbar or sacral spine enters the second stage;
- 2nd degree lumbar osteochondrosis - degenerative disorders and vertebral joint dystrophy occur. The fibrous vertebral ring is pressed, as the nucleus pulposus grows and protrusion (protrusion) of the intervertebral disc occurs.
Neuropathologists determine the second stage of osteochondrosis as lumbago. In other words, lumbago occurs in the lower back when heavy objects are suddenly lifted or with other loads. This period lasts for years, the degree of remission alternating with a worsening acute attack;
- Grade 3 lumbar osteochondrosis - pulp protrusion gradually increases, intervertebral hernia is formed. The patient develops an entire palette of neurological status: persistent pain, irradiation to the back, abdomen, tailbone, legs, urethra, limited movement.
Legends are used to find hernias. The diagnosis of osteochondrosis L5 S1 means that bulging of the nucleus pulposus occurs between the 5th and 1st lumbar vertebrae;
- When therapeutic measures are not taken in a timely manner, all stages of development go smoothly to the next stage. Stage 4 lumbar osteochondrosis is characterized by the development of complications.
As a rule, treatment with drugs for highly advanced pathology is characterized by low efficiency. Neuropathologists are obliged to offer a method of radical action, namely hernia surgery.
Methods for the diagnosis of osteochondrosis
To identify EPP osteochondrosis, a neuropathologist first takes an anamnesis, as patient complaints are one of the determining values for an accurate diagnosis. During the conversation, the patient is asked questions about his health and condition - what and where his pain is, how long it hurts, what strengthens his feelings when stiffness appears, what treatment is done, what treatment is, and the like.

Instrumental diagnostic methods must be used:
- General Rg-graphic images of the lumbar spine- the spine is taken in its entirety or its individual segments are photographed. More often than not, Rg-gram is intended to be made on the basis of complaints, in which doctors are aware of disc atrophy, decreased intervertebral space, osteophyte appearance, smoothing of the lumbar arch;
- Myelography- contrast fluid is injected into the duct where the spinal cord passes through the spinal cord. This technique is used to determine the internal structure of the channel. Ordinary people consider the procedure difficult and dangerous to diagnose, but other than allergy to contrast, puncture of the spinal canal practically does not threaten the patient. Punches are made in places where the spinal cord is absent;
- Computed tomography- nerve root compression, pulp protrusion determined, easy to see vertebral body, ligaments, ducts, soft tissues at close range on monitor;
Most accurately, sacral osteochondrosis is determined using electromagnetic waves, for which the patient is given an examination on a magnetic resonance imaging scanner.
Each tissue has its own input signal, the computer processes the data and displays the picture on the screen. The doctor examines vessels, discs, bone processes, nerve fibers at 1 mm incisions. At the same time, patients do not receive harmful ionizing effects.
Treatment of lumbar spine osteochondrosis
Many patients are interested in the question: what to do with osteochondrosis of the lumbar region? Osteochondrosis of the lumbar spine does not always have clues for surgery. The main thing is that after a thorough examination of the patient, the usual therapeutic measures are sufficient.
Conservative therapy is reduced:
- For drug treatment;
- Physiotherapy procedures;
- Gymnastics exercises from exercise therapy.
Also for the treatment of lumbar spine osteochondrosis, manual therapy methods and methods from traditional medicine are used.
For the treatment regimen of lumbar spine osteochondrosis, surgical methods are offered to patients only in very severe cases, if conservative methods do not give the desired results.
Medicine
Treatment of lumbar spine osteochondrosis is done by a neuropathologist or the narrowest specialist, a vertebrologist. Before treating lumbar chondrosis from a rotating process, the doctor determines the degree and severity of the pathological disorder.
Muscle relaxation is used to relieve pain, reduce cramps, inflammation. These drugs quickly restore mobility to the patient, relieving cramps, until the pain disappears.
In addition to the group of drugs for muscle relaxation, steroid hormones are sometimes used to relieve swelling and inflammation.
Recovery gymnastics
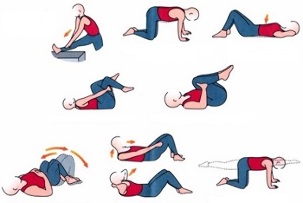
Treatment of lumbar osteochondrosis should be done in conjunction with exercise therapy methods. Exercise and gymnastics should be given the same attention as the use of medications.
The therapeutic effect of osteochondrosis is exercise that relieves pain, strengthens skeletal muscle, reduces compression between discs - this will slow the progression of the disease.
Physiotherapy
In lumbosacral osteochondrosis, treatment involves the use of the following procedures:
- Electrophoresis with drugs;
- Laser and magnetic therapy;
- Treatment with magnetic current;
- Darsonval;
- UV irradiation;
- Treatment diadine;
- Shock wave method.
Manipulation involves the use of methods using natural physical forces: current, light radiation, vibration, and so on. The treatment regimen, the duration of the course for physiotherapy is determined by the attending physician.
Manual therapy
When a sick person asks a neurologist how to cure lumbar spine osteochondrosis using manual techniques, he is usually advised by a qualified specialist who, with his hands, not only affects the muscle tissue, but also puts the vertebrae in place.
In case of lumbar chondrosis, this method normalizes blood and lymph circulation, eliminates muscle tone and deformation, and restores motor function. Chiropractor hand reduces the purity of cramps, reduces back pain.
How is lumbar region osteochondrosis treated using manual techniques and is it possible to fully recover this way? Manual therapy is prescribed only when the degenerative process does not interfere with spinal tissue, i. e. no bone growth is formed. The need for the procedure is determined by the doctor after Rg-diagnostics, CT or MRI.
Surgery
Treatment of lumbar chondrosis with surgery is performed according to specific indications, when the pathology is characterized by the following changes in the spine:
- The spinal canal narrows, the intervertebral disc is compressed and crushed;
- Cauda equina syndrome develops - a large group of spinal nerves, which activate the pelvic, leg, damaged areas;
- Loss of sensitivity increases, there is disruption of the working capacity of internal organs;
- There is a risk of paralysis in the legs.
Operations are carried out according to emergency or planned instructions. The goal of surgical treatment is to relieve stress and improve spinal conditions.
Traditional medicine
Treatment of lumbar spine osteochondrosis with folk methods is best done by consulting your doctor.
People's Pharmacy offers many medicines to cure diseases:

- Medicinal herbs, essential oils, flower extracts, plant roots;
- Animal products, such as snakes or bees, badgers, dogs, lamb fat, boiled eggs and more;
- Iodine, turpentine, and alcohol are used for warming and irritating effects.
Just like medicines, lower back chondrosis is treated by folk methods only in the early stages of the disease, while symptoms are only eliminated, but pathological changes do not disappear. Among other things, such treatments often have side effects, as this requires expert consultation before using recipes from traditional medicine.
Dosage of any folk medicine or medicine should be prescribed by your doctor.
Complications
Lumbar chondrosis in the last stage can lead to unpleasant consequences, including disability.
Against the background of dystrophy and degenerative disorders, narrowing of the spinal canal form, stenosis develops. As a result of these changes, a type of chronic compression is formed, which interferes with normal blood flow, root ischemia or cauda equina syndrome develops.
In addition, sometimes diseases such as spondylosis and spondyloarthrosis develop - intervertebral disc age, loss of strength, and interesting pain appear due to disturbed vertebral joint structure. Complications are most often related to the lower spine, bone-like bone growths form there.
In the third stage, as a complication of osteochondrosis, an intervertebral hernia develops, diseases of the genitourinary system and other internal organs appear.
Precautions
Prevention of lumbosacral spine osteochondrosis is no less important. The lower back has the greatest load, so you need to be careful with the back. Keep in mind that regular gymnastic exercise is the key to a healthy spine.
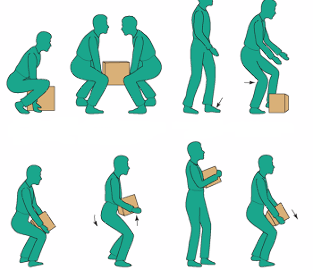
Weight should be lifted very carefully, avoiding sudden jerks. Men and women can carry a reasonable load.
Sitting in the office, you need to monitor your body posture, take proper body posture, and sit in a chair with your back straight. It is good to get up every hour and walk around the room, do squats, twist the torso: this relieves tension throughout the musculoskeletal skeleton.
Trigger point sort is great. They are active or in latent form. Trigger points appear as a result of too much energy, strong stretching, repetitive work, stoop, hypothermia and other factors.
Knowing the causes of the development of spasmodic areas, it is necessary to take steps to exclude its formation. Recently, a trigger point masseuse has gained popularity, it is better to prevent the appearance of painful focus with special tools than to treat it for a long and expensive time.























